Chronic Plantar Fasciitis
Plantar fasciitis is a common and painful foot condition affecting millions of people annually, with approximately 20% of cases becoming chronic. Traditional treatments, such as stretching and medication, work in many but not all situations. The root cause of chronic plantar fasciitis is not inflammation, but tissue degeneration, which challenges the efficacy of anti inflammatory treatments. Surgery is an option but carries risks. Emerging minimally invasive therapies aim to stimulate tissue healing by enhancing local circulation. These include extracorporeal shockwave therapy, radiofrequency microtenotomy, platelet-rich plasma injections, and micromobile compression. Each of these treatments offers an alternative to traditional treatment or surgery for plantar fasciitis, and may help in chronic cases. Targeting the root cause of the ongoing nature of the condition is key. If you suffer from this disruptive affliction, it is suggested that you make an appointment with a podiatrist to discuss whether a minimally invasive therapy may be an option worthy of your consideration.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Dr. Kirk Sherris from Liberty Bay Foot & Ankle. Our doctor can provide the care you need to keep you pain-free and on your feet.
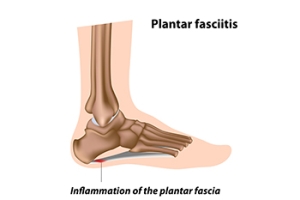
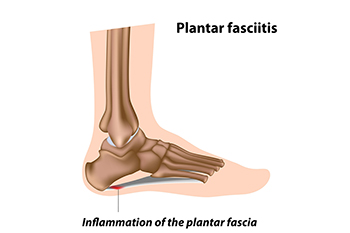
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our office located in Poulsbo, WA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
Harnessing MLS Therapy for Peroneal Pain Relief

Peroneal pain is a common challenge arising from injuries or strain to the lower leg and foot peroneal muscles, often disrupting mobility and well-being. Multiwave Locked System, abbreviated MLS therapy is a groundbreaking technique that offers relief from this discomfort. MLS therapy addresses peroneal pain thoroughly by utilizing synchronized wavelengths of laser light. The continuous wavelength triggers the release of natural pain relievers, swiftly alleviating discomfort, while the pulsed wavelength encourages cellular repair and diminishes inflammation. This dual-pronged approach not only provides relief but also accelerates healing, enabling individuals to regain their stride sooner. The non-invasive nature of MLS therapy ensures minimal disruption to daily life, making it an attractive relief option for peroneal pain. If you have this type of pain, it is suggested that you confer with a podiatrist who can determine if this treatment is right for you.
MLS Laser Therapy is a successful alternative for treating any pain you may be experiencing related to certain podiatric conditions. If you are interested in MLS Laser Therapy, consult with Dr. Kirk Sherris from Liberty Bay Foot & Ankle. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
MLS Laser Therapy
Multiwave Locked System (MLS) Laser Therapy is a patented, FDA-cleared technology that helps relieve pain and inflammation from a number of podiatric conditions, including:
- Heel Pain
- Plantar Fasciitis
- Sports Injuries
- Wounds
- Achilles Tendonitis
- Arthritis
- Neuropathy
- Neuromas
MLS Laser Therapy is an ideal alternative to surgery and prescription medication, as it has no negative side effects and encourages accelerated healing. Among its many clinical benefits, MLS Laser Therapy also:
- Reduces swelling due to bruising or inflammation
- Blocks pain
- Reduces formation of scar tissue
- Improves nerve function
If you have any questions, please feel free to contact our office located in Poulsbo, WA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
MLS Laser Therapy
MLS Laser Therapy is an FDA-approved technology designed to treat various painful conditions. It is often sought out as a successful alternative to surgical treatment and prescription medication that may otherwise bring about negative side effects. During MLS Laser Therapy, light energy enters the damaged cells to stimulate intercellular activity, reducing pain in the affected area and accelerating the recovery process.
MLS Laser Therapy is used in podiatry to treat various conditions. These include heel pain, plantar fasciitis, sports injuries, wounds, Achilles tendonitis, arthritis, neuromas, neurological pain, musculoskeletal disorders, and sore muscles. Aside from the specific conditions MLS Laser Therapy treats, patients can also gain from the treatment’s general benefits. These benefits include a rapid relief of pain, the reduction of swelling caused by inflammation or bruising, faster healing, improved blood circulation, the reduction of scar tissue, and improved nerve function.
MLS Laser Therapy is a non-surgical treatment with no side effects. The treatment process is painless and typically takes a short amount of time to complete. Several treatments may be required depending on the specific condition.
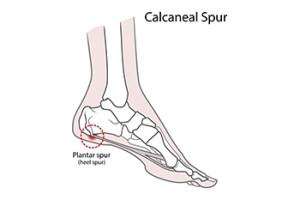
Causes and Symptoms of Heel Spurs
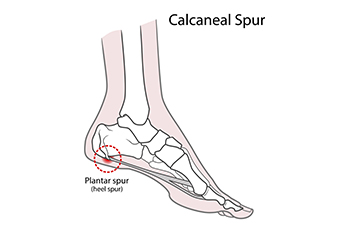
Heel spurs are common, yet often misunderstood, foot conditions that can cause significant discomfort and hinder daily activities. These bony growths develop on the underside of the heel bone and are often associated with plantar fasciitis. The most prevalent symptom of a heel spur is a sharp, stabbing pain in the heel, particularly when taking the first steps after periods of rest. Additionally, prolonged standing or walking can exacerbate the pain. A known cause of heel spurs is the repetitive strain on the plantar fascia, the thick band of tissue connecting the heel bone to the toes. Over time, this strain can lead to inflammation causing the formation of a heel spur. Contributing factors may include wearing improper footwear, obesity, excessive physical activity, or an abnormal foot structure. Early detection and proper treatment are essential for managing the symptoms and preventing further complications associated with heel spurs. If you have heel pain, it is suggested that you consult a podiatrist sooner rather than later for proper treatment techniques.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact Dr. Kirk Sherris from Liberty Bay Foot & Ankle. Our doctor will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact our office located in Poulsbo, WA . We offer the latest in diagnostic and treatment technology to meet your needs.
How to Treat Heel Spurs
Heel spurs are calcium deposits that cause bone protrusions on the heel bone. Heel spurs are usually associated with plantar fasciitis, which occurs when the plantar fasciitis in the foot becomes inflamed. Typically, heel spurs don’t cause any symptoms. However, they can produce chronic or intermittent heel pain. Those who have had the condition often describe the irritation as a stabbing pain.
There are risk factors that may make you more likely to develop heel spurs. People who have abnormal walking gaits, run and jog on hard surfaces, are obese, or wear poorly fitting shoes are more likely to develop heel spurs.
Fortunately, there are precautions you can take to avoid developing heel spurs. One of the best ways to do this is by wearing well-fitting shoes with shock-absorbent soles. Another preventative technique is to choose running shoes if you plan on running, and walking shoes if you plan on walking. Shoes are made for different activities and it is important to research a shoe before you purchase a pair.
The pain associated with heel spurs often decreases the more you walk. However, a recurrence of pain after an extended period of rest or walking is likely to occur with this condition. Those with severe heel spur pain may opt to go the surgical route for treatment. However, more than 90% of those with the condition get better without surgical treatment. If you have a heel spur and want to know if surgery is right for you, you should go to your podiatrist and he or she will be able to conduct a pre-surgical test or exam to determine if you are an optimal candidate for surgery.
How to Deal with Athlete's Foot
Athlete’s foot is a type of fungal infection that affects the skin on the feet. It is caused when the tinea fungus grows on the foot. It is possible to catch the fungus through direct contact with someone who has it or by touching a surface that is contaminated with it. This type of fungus thrives in warm, moist environments such as showers, locker room floors, and swimming pools. Your risk of getting it may also increase by wearing tight-fitting, closed-toe shoes, or by having sweaty feet.
Symptoms of athlete’s foot include itching, stinging or burning sensations between the toes. You may also experience toenails that are discolored, thick, crumbly, or toenails that pull away from the nail bed.
Your podiatrist may diagnose athlete’s foot by detecting these symptoms or by doing a skin test to see if there is a fungal infection present. The most common exam used to detect Athlete’s foot is a skin lesion potassium hydroxide exam. To use this method, your doctor will scrape off a small area of the infected skin and place it into potassium hydroxide. The potassium hydroxide will destroy the normal cells and leave the fungal cells untouched so that they are visible under a microscope.
There are a variety of treatment options for athlete’s foot. Some medications are miconazole (Desenex), terbinafine (Lamisil AT), clotrimazole (Lotrimin AF), butenafine (Lotrimin Ultra), and tolnaftate (Tinactin). While these options may be able to treat your fungus, it is best that you consult with a podiatrist in order to see which treatment option may work best for you.
In some cases, Athlete’s foot may lead to complications. A severe complication would be a secondary bacterial infection which may cause your foot to become swollen, painful, and hot.
There are ways that you can prevent athlete’s foot. Washing your feet with soap and water each day and drying them thoroughly is an effective way to prevent infections. You also shouldn’t share socks, shoes, or towels with other people. It is crucial that you wear shower sandals in public showers, around swimming pools, and in other public places. Additionally, you should make sure you wear shoes that can breathe and change your socks when your feet become sweaty. If you suspect that you have Athlete’s foot, you should seek help from a podiatrist as soon as possible.
Are Bunions Affecting Your Everyday Life?
Minor Wound Care Methods

A wound is defined as damage to the skin’s surface. Wounds occur when there is a break in the skin due to a cut or scrape. A wound can also be caused by an animal bite and bedridden patients may develop bed sores. For mild wounds, proper wound care can begin with washing the hands, followed by holding a clean cloth on the affected area to help stop the bleeding. It is beneficial to rinse the wound with water and remove any dirt that has lodged inside of it. When the wound is dried, a bandage or gauze can be used to cover it. It is beneficial to change the dressing daily which may help to keep it free of bacteria that may accumulate from daily activities. If you have a wound on your foot, it is strongly suggested that you speak with a podiatrist who can treat and monitor the severity of the wound.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Dr. Kirk Sherris from Liberty Bay Foot & Ankle. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Poulsbo, WA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Blog Archives
- May 2025
- April 2025
- March 2025
- February 2025
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019